156 million Americans get health benefits from their employer at a shared cost to employees and employers. On average these shared costs add up to more than 25% of the employee’s base pay. That’s a lot of money spent by both the employee and employer for benefits.
We work with 45% of all Fortune 500 as well as countless smaller employers to help employees get the most from those benefits. If there’s one thing that I can say with certainty it's that it can be really frustrating when our customers invest in great benefits that go to waste. It means that employees don’t get the care that they deserve and their out of pocket costs go up. For the employer, costs go up as do other metrics, like absenteeism.
The challenges of getting members to engage with their health care benefits are countless and well documented. Even the most advanced benefits teams struggle with the complexity of member communications as well as low health care & finance literacy. Regulations make communications difficult and, and, and - the list goes on.
But here’s the thing: The reason benefits go under-utilized is not just because of these well known obstacles. There’s also something larger at play and it’s this - the world has fundamentally changed and benefits communications strategy hasn’t kept up.
When I’m asked to present my company’s engagement capabilities to an employer, one of the things I do is show a picture of a Google search and ask: “How many people in this room have searched about a health topic in the last year?”
Everyone raises their hand, (including me). So while it’s clearly important to have great benefits and a hub for employees to find them, it’s only part of the solution. It’s only part of the solution because even people in the business of benefits aren’t going to their own benefits site first, including me. Finding health care information in places other than the employer’s benefit communications channels is now the norm, not the exception.
This transition has profound implications for how people make decisions about their health. As popular online sources of health information have expanded, their purity has noticeably diminished.
Take a look at the Google search results for “Sore Back” above, do you notice anything funny about it?
The first link you see is from Mayo Clinic, a credible site. The second link you see is from WebMD, also credible. Both of these sites have a clinical review process so they are the kind of sites we’d hope our members consult before making a health care decision, right?
Here’s the rub. When you click on the Mayo site link, the CTA (call to action for you non-marketers) is to motivate you to schedule an appointment. Move your attention to the image below and take a look at the WebMD site. You get solid, clinically reviewed information, completely surrounded by advertisements for Humira, a specialty drug.
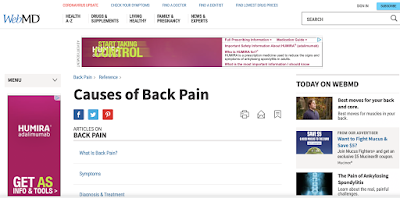
So even your most well informed member who went to a credible site was steered in a direction that may not be his or her best bet for their initial sore back inquiry.
20 years ago, health care information was much less accessible. In 2000, only 4% of US households had broadband and WebMD was just a few years old. If you wanted to find health care information, you asked friends, you asked your doctor, and you looked at what came in your benefits package.
Times have changed. Today members start their searches with Dr. Google, WebMD, HealthGrades, and many other health sites. In addition, they read articles on the New York Times, in their fitness apps, in digital newsletters, and from hundreds of other less reputable publishers.
But let’s not forget the impact of aggressive advertising tactics used by companies similar to what we just witnessed. Commercial interests ranging from pharmaceutical companies, to gyms and fitness companies, health food companies, to nutraceutical purveyors are all vying to get their product in front of the health care consumer. And unlike 20 years ago when it was hard to get the data, segment the consumer and expensive to target and reach her, today it’s much easier and less expensive.
So to sum it up, you could say that advertisers often have better access to the health care consumer than even the most successful benefits teams. The world of consumer communications has changed and benefits communications have had a hard time keeping up. And for good reason.
Implementing great consumer marketing involves micro-targeting, which takes resources and a lot of data. And while benefits teams often have an eligibility file and maybe even email addresses, they often don’t have the extensive resources that consumer marketers have. Resources such as a massive treasure trove of data with hundreds of fields for each member informing the best offer, message, and channels that will take the consumer from inaction to action.
The question is, if a commercial interest is doing the best, data-driven marketing, is your employee getting good decision support to drive the right action?
Employees sometimes develop trust issues with their employer. They don’t want the employer knowing too much about their health care or may think their employer is motivated only by cutting costs. What they don’t realize is how much data is available about them online to organizations with less interest in their wellbeing than the employer. Increasingly, consumer marketing companies can use large amounts of non-PHI data to infer health information - to offer products and services.
Having worked with many, many employers of all stripes, I can tell you that most are aligned with the same goals as their members: better health care with lower costs. These goals are beneficial for both the employee and the employer. It’s a simple alignment that should move both parties in the right direction.
So with employers and employees aligned on these critical goals, what’s the problem?
Advertisers and the publishers who enable them don’t have the same goals as employers and consumers. They are focused on clicks and revenue not health and lower costs. It’s for this reason that even when a member looks at a well vetted health site or at an article that’s been through clinical review, they’re probably seeing an advertisement for a drug or other remedy that may not be the best choice for their situation.
It’s in this moment when the member searches for relief from a sore back and gets decision support from an advertiser that she chooses to go to an ER rather than an urgent care facility, or decides to call a surgeon rather than try an ice pack. And the reality is that these decision-support failure moments happen every minute of every day.
So what can we do to provide better decision support to health care consumers? I have an idea that is coming in another blog. It involves technology, data, and content. I talked about some elements of the plan here, but to really make it happen we’ll need to do a lot more.
What do you think?
We work with 45% of all Fortune 500 as well as countless smaller employers to help employees get the most from those benefits. If there’s one thing that I can say with certainty it's that it can be really frustrating when our customers invest in great benefits that go to waste. It means that employees don’t get the care that they deserve and their out of pocket costs go up. For the employer, costs go up as do other metrics, like absenteeism.
The challenges of getting members to engage with their health care benefits are countless and well documented. Even the most advanced benefits teams struggle with the complexity of member communications as well as low health care & finance literacy. Regulations make communications difficult and, and, and - the list goes on.
But here’s the thing: The reason benefits go under-utilized is not just because of these well known obstacles. There’s also something larger at play and it’s this - the world has fundamentally changed and benefits communications strategy hasn’t kept up.
When I’m asked to present my company’s engagement capabilities to an employer, one of the things I do is show a picture of a Google search and ask: “How many people in this room have searched about a health topic in the last year?”
Everyone raises their hand, (including me). So while it’s clearly important to have great benefits and a hub for employees to find them, it’s only part of the solution. It’s only part of the solution because even people in the business of benefits aren’t going to their own benefits site first, including me. Finding health care information in places other than the employer’s benefit communications channels is now the norm, not the exception.
This transition has profound implications for how people make decisions about their health. As popular online sources of health information have expanded, their purity has noticeably diminished.
Take a look at the Google search results for “Sore Back” above, do you notice anything funny about it?
The first link you see is from Mayo Clinic, a credible site. The second link you see is from WebMD, also credible. Both of these sites have a clinical review process so they are the kind of sites we’d hope our members consult before making a health care decision, right?
Here’s the rub. When you click on the Mayo site link, the CTA (call to action for you non-marketers) is to motivate you to schedule an appointment. Move your attention to the image below and take a look at the WebMD site. You get solid, clinically reviewed information, completely surrounded by advertisements for Humira, a specialty drug.
So even your most well informed member who went to a credible site was steered in a direction that may not be his or her best bet for their initial sore back inquiry.
20 years ago, health care information was much less accessible. In 2000, only 4% of US households had broadband and WebMD was just a few years old. If you wanted to find health care information, you asked friends, you asked your doctor, and you looked at what came in your benefits package.
Times have changed. Today members start their searches with Dr. Google, WebMD, HealthGrades, and many other health sites. In addition, they read articles on the New York Times, in their fitness apps, in digital newsletters, and from hundreds of other less reputable publishers.
But let’s not forget the impact of aggressive advertising tactics used by companies similar to what we just witnessed. Commercial interests ranging from pharmaceutical companies, to gyms and fitness companies, health food companies, to nutraceutical purveyors are all vying to get their product in front of the health care consumer. And unlike 20 years ago when it was hard to get the data, segment the consumer and expensive to target and reach her, today it’s much easier and less expensive.
So to sum it up, you could say that advertisers often have better access to the health care consumer than even the most successful benefits teams. The world of consumer communications has changed and benefits communications have had a hard time keeping up. And for good reason.
Implementing great consumer marketing involves micro-targeting, which takes resources and a lot of data. And while benefits teams often have an eligibility file and maybe even email addresses, they often don’t have the extensive resources that consumer marketers have. Resources such as a massive treasure trove of data with hundreds of fields for each member informing the best offer, message, and channels that will take the consumer from inaction to action.
The question is, if a commercial interest is doing the best, data-driven marketing, is your employee getting good decision support to drive the right action?
Employees sometimes develop trust issues with their employer. They don’t want the employer knowing too much about their health care or may think their employer is motivated only by cutting costs. What they don’t realize is how much data is available about them online to organizations with less interest in their wellbeing than the employer. Increasingly, consumer marketing companies can use large amounts of non-PHI data to infer health information - to offer products and services.
Having worked with many, many employers of all stripes, I can tell you that most are aligned with the same goals as their members: better health care with lower costs. These goals are beneficial for both the employee and the employer. It’s a simple alignment that should move both parties in the right direction.
So with employers and employees aligned on these critical goals, what’s the problem?
Advertisers and the publishers who enable them don’t have the same goals as employers and consumers. They are focused on clicks and revenue not health and lower costs. It’s for this reason that even when a member looks at a well vetted health site or at an article that’s been through clinical review, they’re probably seeing an advertisement for a drug or other remedy that may not be the best choice for their situation.
It’s in this moment when the member searches for relief from a sore back and gets decision support from an advertiser that she chooses to go to an ER rather than an urgent care facility, or decides to call a surgeon rather than try an ice pack. And the reality is that these decision-support failure moments happen every minute of every day.
So what can we do to provide better decision support to health care consumers? I have an idea that is coming in another blog. It involves technology, data, and content. I talked about some elements of the plan here, but to really make it happen we’ll need to do a lot more.
What do you think?